
We report the case of a patient with antineutrophil cytoplasmic antibody ANCA-associated vasculitis with involvement of the temporal artery presenting with clinical manifestations of giant cell arteritis and temporal arteritis such as temporal headache jaw claudication weight loss night sweats and increased inflammatory parameters. 29200154 Indexed for MEDLINE Publication Types.
Associated complaints may include.
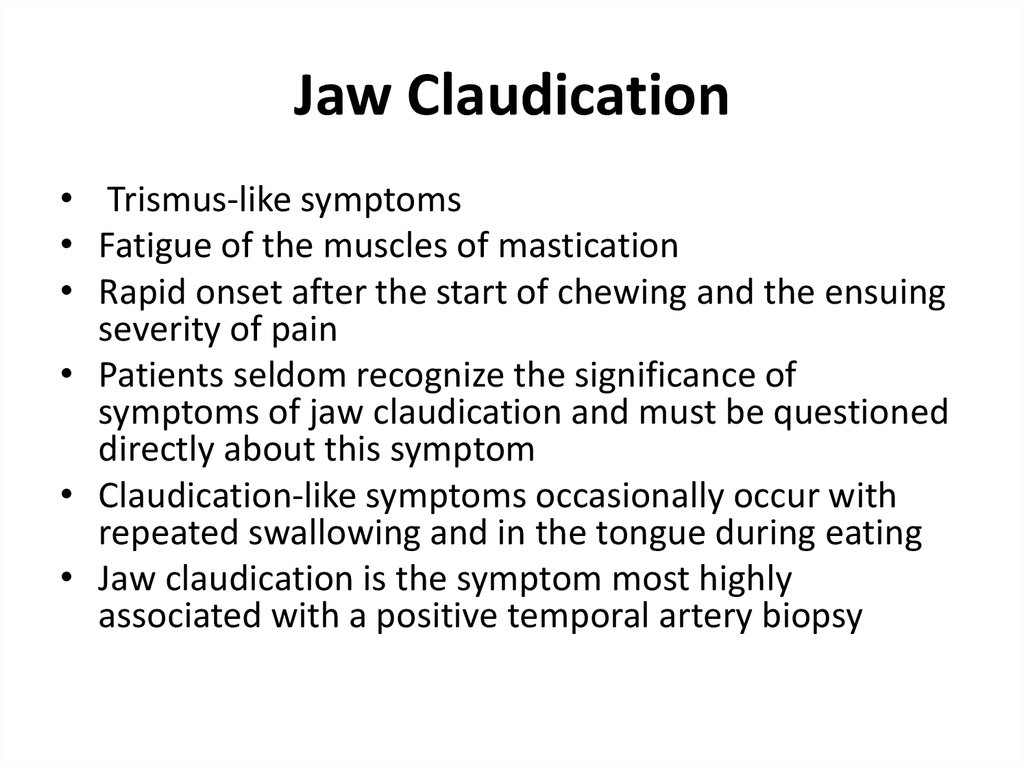
Jaw claudication differential diagnosis. Jaw claudication is pain in the jaw associated with chewing. It is a classic symptom of giant-cell arteritis 1 2 but can be confused with symptoms of temporomandibular joint disease rheumatoid arthritis of the temporomandibular joint myasthenia gravis tumors of the parotid gland or occlusion or stenosis of the external carotid artery. Jaw claudication is an often unrecognized sign of giant cell arteritis.
The significance of this symptom has been underemphasized in the dental literature. Dentists should consider jaw claudication when making the differential diagnosis of jaw pain especially in the elderly patient. Early diagnosis and treatment of giant cell arteritis may help save a patients vision.
Although an algorithm for diagnosing GCA that includes both biopsy and imaging examinations has been recently proposed it harbors the possibility of false negatives. Hence jaw claudication caused by ischemia of the masticatory muscles is one of the important clinical predictors for implementation of temporal artery biopsy TAB. Average age at the time of diagnosis 30 yrs Pseudotumor Cerebri IIH CC.
Pounding intermittent HA w increasing severity. Usually worse in the am and precipitated by changes in posture. Associated complaints may include.
Decreased vision Transient visual obscurations lasting seconds Diplopia horizontal Dizziness Tinnitus. The British Society for Rheumatology guideline Mackie 2020a states that headache scalp tenderness jaw claudication visual loss and stroke are all cranial manifestations of giant cell arteritis GCA. Inflammation of the aorta andor its proximal branches is also common in GCA and may be asymptomatic or present with non-specific systemic symptoms such as fever or weight loss.
Typical symptoms of PMR include aching and stiffness in the shoulders and proximal limb muscles with or without mild polyarthritis or tenosynovitis. Although GCA and PMR frequently co-exist cranial symptoms including headache jaw claudication and vision symptoms are typically absent in patients with PMR. PMR typically has less prominent symptoms than GCA.
Typical symptoms of PMR include aching and stiffness in the shoulders and proximal limb muscles with or without mild polyarthritis or tenosynovitis. Although GCA and PMR frequently coexist cranial symptoms including headache jaw claudication and vision symptoms are typically absent in patients with PMR. PMR typically has less prominent symptoms than GCA.
We report the case of a patient with antineutrophil cytoplasmic antibody ANCA-associated vasculitis with involvement of the temporal artery presenting with clinical manifestations of giant cell arteritis and temporal arteritis such as temporal headache jaw claudication weight loss night sweats and increased inflammatory parameters. The ultrasound scan showed a typical halo sign of the temporal artery. Characteristic findings include headache jaw claudication visual loss and constitutional symptoms malaise fever weight loss loss of appetite.
Localized GCA symptoms are the end-result of vascular insufficiency and tissue ischemia. Temporal artery biopsy TAB remains the gold standard for diagnosis. Additional diagnostic tests include blood tests erythrocyte sedimentation rate ESR.
This case suggests that RCM can cause temporal artery thrombosis and should be considered as a differential diagnosis in severely immunocompromised patients with maxillary sinusitis presenting with jaw claudication. 29200154 Indexed for MEDLINE Publication Types. Differential diagnosis Vascular or arterial claudication typically occurs after activity or ambulation for a distance with resultant vascular insufficiency lack of blood flow where the muscular demands of oxygen outweighs the supply.
Symptoms are lower extremity cramping. The diagnostic processes to clarify the diagnosis of 7th nerve pain is as varied as the origins of the disorder. Indium 111 scan to look for infection in the sinus region or roots of the teeth.
This is more reliable than an anatomical test such as a dental X-ray. An MRI of the brain to look for space occupying lesion in the brain which could push on the 7th nerve. Once the cause is thought to be infective then.